The Federal Trade Commission (FTC) recently announced that it would seek to block Amgen’s proposed $27.8 billion acquisition of Horizon Therapeutics. The move was the culmination of several years’ worth of increased scrutiny from both Congress and the FTC into antitrust issues in the biopharmaceutical industry. While the FTC’s move didn’t elicit much public comment, it raised considerable alarm in various corners of the biopharmaceutical industry—specifically, that it would chill beneficial biopharmaceutical M&A activity.
This piece, which aims to shed light on the FTC’s theory of the harm in the case and its consequences for the industry, will be divided into two parts. This first post will discuss the overall biopharmaceutical market and the FTC’s stated theory of harm. In a subsequent post, I will dive more deeply into the economic theories that underpin the case and the risk-benefit tradeoff inherent in the FTCs decision to challenge the merger.
The Biopharmaceuticals Market and the Importance of M&A
Amgen is one of the world’s largest biopharmaceutical firms, with 2022 sales of $24.8 billion. The firm’s origins date back to the 1980s, but in the decades since, it has transformed from a biotechnology startup focused on manufacturing recombinant proteins for use as drugs into a diversified pharmaceutical leader. Its current sales are mostly generated by a portfolio of nine blockbuster drugs that each earn more than $1 billion in annual sales, the most important of which are:
-
- Enbrel (etanercept), which is used to treat a wide variety of autoimmune diseases;
-
- Prolia (denosumab), which is used to treat osteoporosis in elderly patients; and
-
- Otezla (apremilast), which is also used to treat autoimmune diseases, most notably psoriatic arthritis.
Horizon Therapeutics, on the other hand, is a small biopharmaceutical firm that got its start in a relatively mundane manner: combining multiple generic drugs into a single tablet. Horizon’s strategy shifted over time, however, with the firm seeking to purchase undervalued therapeutics from bankrupt pharmaceutical companies and then re-launch them. This strategy yielded the two drugs that the FTC’s case focuses on:
-
- Tepezza (teprotumumab-trbw), which the company acquired in 2017 and treats the eye disease that is seen with Grave’s Disease, a form of hyperthyroidism; and
-
- Krystexxa (pegloticase), which the company acquired in 2015 from a private-equity company and which is used to treat gout that has not responded to other “first-line” medications.
At first glance, the FTC’s decision to challenge this merger might seem relatively uninteresting—certainly not an action that would warrant the alarm that has been generated in the biopharmaceutical community. The industry’s concern makes more sense, however, when one appreciates the crucial role that mergers and acquisitions have come to play in the biopharmaceutical innovation process.
First, it’s worth stating that the kinds of acquisitions that have become an important part of the biopharma R&D ecosystem are not large horizontal mergers between existing biopharmaceutical companies. Examples of the latter include the Bristol-Myers-Squibb – Celgene merger in 2018, and the Merck-Wyeth merger of 2009. Rather, it is smaller acquisitions—in which large biopharmaceutical firms acquire small biopharmaceutical firms with no approved drugs, or at most one or two recently approved drugs—that are the focus.
Some data would be helpful to illustrate the scale of this type of activity and its importance to biopharmaceutical innovation. Biopharmaceuticals are an M&A-intense industry. In 2021, the industry engaged in 196 transactions worth $152 billion—more than any other U.S. industry. Moreover, this M&A activity is tightly linked to research and product development in ways that M&A activity in other industries simply isn’t.
For example, in 1997, the contribution of drugs that were “acquired” to the sales of large pharmaceutical firms was a mere 10%. That is, 90% of branded pharmaceutical revenue was sourced from drugs that pharmaceutical firms invented “in house.” Today, that number is just 37%, with 73% of revenue originating either from acquisitions of small companies or “partnered” deals with small companies. An analysis from McKinsey concurs, noting that “66 percent of the entire industry’s pipeline revenues were generated from [externally sourced drugs].” Another study performed in the early 2010s showed that of the roughly 170 new drugs approved by the FDA from 2011 to 2016, about 65% were originally discovered by smaller firms before being bought by larger pharmaceutical firms who continued to develop the drugs and bring them to market. (See also here, here, and here.)
Each of these datapoints come together to tell a very clear story. Specifically, over a period of about 20 years, the biopharmaceutical R&D model shifted from one in which established large pharmaceutical companies conducted every step in the drug-development value chain to one in which large firms have “outsourced” earlier steps in the R&D chain and concentrated their activities on running the large “Phase 3” trials that are needed to indisputably prove a drug’s efficacy.
Some have attempted to use this shift to paint large pharmaceutical firms as “uninnovative,” but it’s important to note that there are many reasons to believe that this specialization is likely to be efficient. Not only do economists generally tend to agree that specialization enhances productivity, but there’s also early evidence to verify this conclusion empirically in the context of pharmaceuticals, as compounds that are “partnered” (i.e., discovered by a different firm than the one that ultimately brings them to market) have a much higher probability of success than unpartnered compounds.
Taken together, the importance of M&A to the biopharmaceutical innovation engine should not be understated.
The FTC’s Theory of Harm
Given the importance of small-company M&A to biopharmaceutical innovation, why is the FTC challenging the Amgen-Horizon merger? Simply put, the FTC believes that, after the acquisition, Amgen will engage in a business practice known as “bundled rebates” in which it “provides greater rebates on one or more of its blockbuster products to secure favorable formulary placement for other medications in different product markets.” The commission believes this will “block smaller rivals from being able to compete on the merits.”
Specifically, the FTC argues that Amgen will provide discounts to pharmaceutical benefit managers (PBMs) on its broad set of existing products, like Enbrel, Prolia, and Otezla, in order to secure preferred formulary placement for the new drugs it is acquiring from Horizon, including Tepezza and Krystexxa. This, the argument goes, would thereby exclude any rising competitors to those drugs and thus harm consumers.
Rebates or discounts are a feature of nearly all markets, but they play a special role in the biopharmaceutical industry. In the United States, rebates are negotiated by PBMs, whose function is to define formularies on behalf of health insurers. These formularies are essentially “lists” of which medications an insurance plan is going to cover, the price the insurer will pay the manufacturer for each drug, and how much of each drug’s price is going to come out of the patient’s pocket. The “price” that is negotiated comes in the form of the aforementioned rebates off the drug’s “list” price. For example, a PBM and a pharmaceutical manufacturer might negotiate and end up settling on a 10% rebate off of a list price of $1,000 a dose, leading to a “net price” of $900 a dose. In essence, the PBM functions as a contracted agent to negotiate prices with pharmaceutical manufacturers on the behalf of the insurers, and the rebate governs the net price the insurer ends up paying the pharmaceutical company.
The broader question of the social utility of this rebate system has been ongoing for years. Supporters claim that the system helps to rein in drug spending by forcing pharmaceutical firms to offer rebates to secure formulary placement. Detractors argue that it is responsible for a growing “net-list price bubble,” in which list prices are artificially inflated to provide rebates to PBM customers, without any gain to insurers or patients in the form of lower premiums.
This debate has now spilled into policy discussions, with both regulators and Congress increasing their scrutiny of the rebate process. For example, Congress asked the FTC to investigate the PBM industry and the rebate process back in July 2020, and the FTC responded with both a 2021 report and a 2022 policy statement in which it voiced its concerns both the broader rebate process. While the FTC was broadly critical of the rebate process, however, it singled out a specific type of rebate practice that it would investigate even more closely: the selective use of rebates to foreclose competition from alternative drugs. This is the same practice that the FTC has centered on in its case against Amgen.
Rebates have also recently emerged as the focus of several private antitrust case. Among the two most significant was a 2016 complaint by Pfizer alleging that claimed that Johnson & Johnson—the maker of Remicade, a best-selling medication for autoimmune disease—threatened not to pay rebates to PBMs unless they excluded from their formulary Pfizer’s biosimilar imitator to Remicade: Inflectra. According to Pfizer, this limited Inflectra’s market share to just 4%.
Even more relevant to the Horizon merger is a 2022 lawsuit filed by Regeneron against Amgen that accused it of providing rebates on Otezla and Enbrel to secure preferred formulary status of its own PCKS9-inhibiting drug Praulent over Regeneron’s competing drug Repatha. This claim is identical to the one that the FTC makes today, and is referenced by the FTC itself in its filing.
Taken together, the intense regulatory scrutiny and private antitrust litigation surrounding the topic of bundled rebates in biopharmaceuticals warrants a detailed discussion of their economic effects.
Conclusion
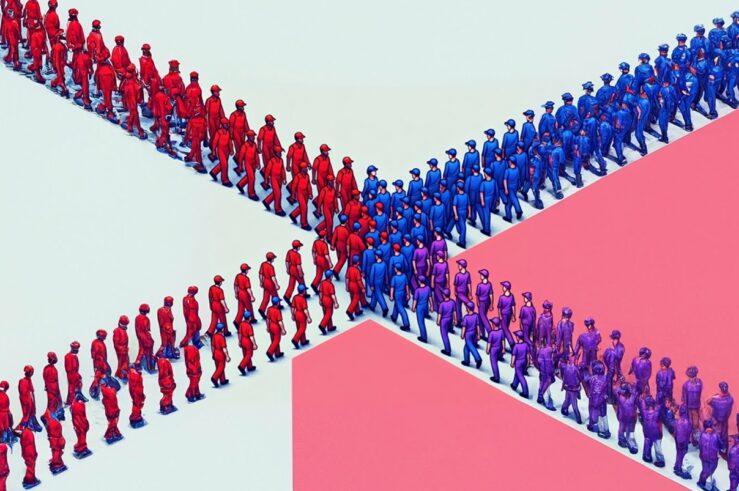
Against this backdrop, the stage is set for a landmark antitrust case. On one side stands the pharmaceutical industry, long accustomed to a relatively permissive M&A environment that has allowed it to engage in specialized technology acquisition, buying small companies to acquire promising new drugs before pushing them across the finish line through large Phase 3 trials. On the other side stands the FTC, eager to demonstrate that these mergers might not be so benign as once thought.
Looming over both parties is the rise of the rebate process and the controversy it has engendered. In Part II, I will perform a detailed review of the economic theories and data that might be applicable to this landmark case.