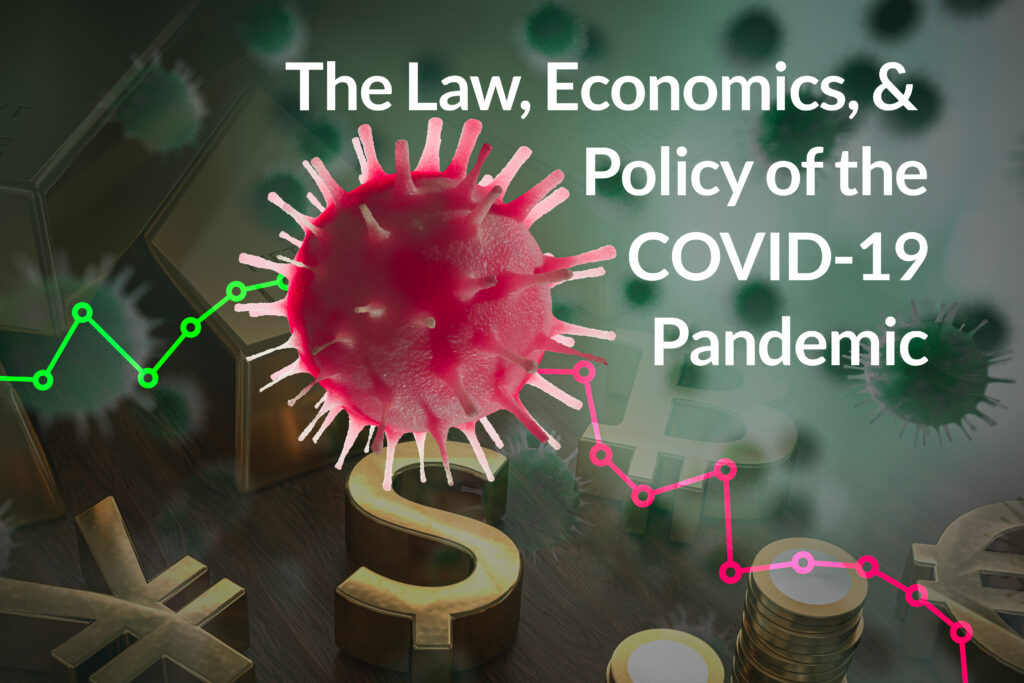
The brutal toll of the coronavirus pandemic has delivered dramatic public policies. The United States has closed institutions, banned crowds, postponed non-emergency medical procedures and instituted social distancing. All to “flatten the curve” of illness. The measures are expensive, but there is no obvious way to better save lives.
There is evidence that, even without the antivirals or vaccines we hope come soon, we are limiting the spread of COVID-19. Daily death totals for the world appear to be leveling; the most severely impacted countries, Italy and Spain, are seeing declines; the top U.S. hotspot, New York, appears to be peaking (and net new coronavirus hospital admissions fell substantially yesterday). I hope that, looking back, these inferences look reasonable.
But of course I do. Is that rational introspection, or confirmation bias? To try to know, we should look about to see how others are addressing this challenge, and how well they are doing. There are experiments being run, in real time on actual economies, and diversity of results is one of the few blessings conveyed by our coronavirus demon.
Differing approaches to mitigating externalities around the world
It strikes many as entirely off-topic to discuss the efficiency of our measures, as though only the most expensive, draconian remedies work. There is a tendency to stress how little room for optionality there exists. Exhortation seems to be the strategy. No doubt, we are confronted by a classic “public good” challenge, where individuals may impose costs on others. Not intentionally, but perhaps through actions that are short-sighted. If a neighbor fails to take “due care” they needlessly endanger others. To overcome such free riding, we “rally ‘round the flag” to condemn anti-social behavior. That is a community survival trait.
And entirely compatible with the pursuit of efficient rules. Shuttering the marketplace and freezing personal mobility imposes harsh hardships; they are, unsurprisingly, resisted. It is stunning how rapidly our Conventional Wisdom has changed, but as recently as January 29 N.Y. Times’ tech columnist Farhad Manjoo warned us to slow down, to “Beware the Pandemic Panic.” He echoed the World Health Organization’s view that the threat was meek and that we ought focus on “not the illness itself but the amped-up, ill-considered way our frightened world might respond to it.” (See Jonathan Tobin’s nice overview of the errors made, left and right, in the run-up to the lock-down. It notes Manjoo’s reversal in the Times, Feb. 26.)
When the disease seemed less, we were reluctant to impose costs; as the threat loomed larger, we rushed to make up for lost time. We now pay the price for acting late, but without perfect foresight – our perennial state – that insight does not much help us today or prep us for tomorrow. Keen observation of more efficient ways, and robust public discussion, will.
Sweden has adopted the hygiene and separation practices familiar to Americans. But the government has stopped short of mandates imposed elsewhere. While college courses have rolled over to the Internet, Sweden has not closed schools for students 16 and under. Bars and restaurants remain open, with gatherings up to 50 approved (the US President has asked crowds to be kept to 10 or less). Life seems almost normal to many – Americans might pay a ton for that. Still, substantial macroeconomic costs remain. One estimate predicts a 4% decline in 2020 GDP, beating expectations for Europe but similar to U.S. forecasts (see Goldman Sachs’ March 26 report with 2020 U.S. GDP growth projection of -3.8% and -9% for European markets.) Alas, the Swedish fatality rate, population adjusted, is higher than its Scandinavian peers and (as of April 7) about one-half higher than the U.S. See Table.
COVID-19 Fatality Rates per Million Population, Selected Countries (4.7.20)
| Country | Deaths/mil. | Days since 1/mil. | Daily Growth | Geo. Avg. Weekly Growth/day |
| USA | 38.6 | 16 | 1.18 | 1.19 |
| Italy | 284.3 | 35 | 1.04 | 1.05 |
| Spain | 298.2 | 27 | 1.05 | 1.08 |
| Czech Rep. | 8.2 | 10 | 1.13 | 1.16 |
| Sweden | 57.2 | 19 | 1.24 | 1.19 |
| Switzerland | 95.6 | 25 | 1.07 | 1.10 |
| U.K. | 92.9 | 20 | 1.15 | 1.19 |
| France | 154.2 | 25 | 1.16 | 1.17 |
| Germany | 24.2 | 17 | 1.11 | 1.15 |
| Singapore | 1.1 | 3 | 1.0 | 1.0 |
| S. Korea | 3.7 | 29 | 1.03 | 1.02 |
| Japan | n/a | n/a | n/a |
Source: https://91-divoc.com/pages/covid-visualization/
The Czech Republic – with a much lower COVID-19 mortality rate – innovated. The Czechs imposed the standard hygiene and social distancing practices, but added a twist: every person, when in public, is obligated to wear a face mask. It need not be medical grade. This sidestep not only spares supplies for crucial medical professionals, who work in close proximity to patients infected with coronavirus, it has unleashed a popular movement to sew home-made masks. That has jump-started social norms to reduce infections by wearing protective gear. And its simple logic is compelling: you protect me, I protect you.
Of course, the masks do not block one hundred percent of potential transmissions – perhaps no more than two-thirds, under favorable conditions, according to a 2013 study in the journal Disaster Medicine and Public Health Preparedness, Testing Homemade Masks for Efficacy: Would they Protect in an Influenza Pandemic?. The findings, showing results for filtering effectiveness using different materials masks, are given in the Table below. They suggest that (a) no masks are perfectly effective in blocking all tiny particles, including infectious biological matter; (b) surgical masks are relatively effective; (c) homemade masks are less effective, but much better than nothing – and should be used in conjunction with other (distancing, hygiene, etc.) practices. Where surgical masks are too expensive or unavailable, cotton face masks (sewn with multiple layers) or vacuum bags (if you can snag them) are useful substitutes. Their role is to suppress rates of disease progression, bending the curve and managing the pandemic.
The decision to encourage and then require masks (with an order effective midnight March 18) led to an enthusiastic campaign to make stylish, personalized gear – soon posted on Insta. It channeled the desire of citizens to both battle coronavirus and yet to continue living their lives. Mask wearing then further served as a reminder to observe additional rules of separation, while discouraging people from touching their face. A video on the virus went viral. It’s beautifully logical and upbeat, as global emergency crisis responses go. Judge for yourself.
No doubt more research should be performed; an entire industry of PhD theses from epidemiology to sociology to public health may homestead this topic in the post-Coronavirus world. But we also must pay attention to our experimental results in real time. The Demonstration Effect is, and should be, powerful. Countries such as Slovakia and Belgium saw the Czech Republic’s approach, relative openness (low-cost mitigation), and superior survival rates, and quickly adopted similar policies.
The U.S. rationale for discouraging mask use
U.S. policy makers initially shielded themselves from the face mask question by issuing the “institutional no.”[1] The American public was instructed by the Center for Disease Control (CDC) to refrain from wearing masks save in the instance where they were infected. There were three reasons. First, that wearing masks would actually harm healthy people not impacted with COVID-19. Second, the masks were ineffective in shielding small aerosol particles, particularly since non-professionals would not wear them properly. Third, the limited supply of high-quality, medical grade face masks should be reserved for doctors, nurses, and other health care workers who, by the nature of their tasks, could not observe “social distancing” or otherwise avoid infected COVID-19 patients.
The third rationale had an advantage over the first two as not being false. But by the logic used to prioritize medical professional mask protections, buttressed by a modicum of public education, the rest of us would be likely to benefit, as well. The CDC was arguing magnitude and rankings (OK), and then configuring the effectiveness arguments to justify the rankings (not OK). It was a blunder, squandering precious time and undercutting agency credibility. Moreover, the administrative edict pretended to be scientific when it was crafting (bad) economics. The Czechs and many Asian countries discovered (as disaster preparedness research had already found) that ad hoc masks work reasonably cheaply, quickly and well, and that the population can be protected to a non-trivial degree by producing their own. No need to steal N-95 respirators from frontline warriors; we’ll just make more (lower quality) protection devices.
Tip your cap to the Czech Republic. The story busted out. On March 30, The Guardian wrote: “Czechs get to work making masks after government decree: Czech Republic and Slovakia are only countries in Europe to make coronavirus mask-wearing mandatory.” By April 2, Dr. Ronald Depinho, a former president of M.D. Anderson, was editorializing: “Every American should wear a face mask to defeat Covid-19.” His empirical take was informed by a graphic (popularly Tweeted) showing fatality rates across countries – in general, the mask wearing societies of Asia (Japan, South Korean, Singapore, Taiwan) were seen to be doing relatively well in limiting the COVID-19 carnage.
Face Masks As Pandemic Defense (4.2.20) Source: STAT
Human experiments are often considered cruel. But when they are run, let us learn from them.
U.S. about-face on mask use
And so the U.S. policy flipped. As per TIME:
On April 3, President Trump announced that the CDC now recommends that the general population wear non-medical masks—meaning fabric that covers one’s nose and mouth, like bandanas or cut T-shirts—when they must leave their homes to go to places like the grocery store. The measure is voluntary. The mayors of Los Angeles and New York City have already made similar recommendations. In other parts of the country, it’s not voluntary: for example, officials in Laredo, Texas have said they can fine people up to $1,000 when residents do not wear a face covering in public.
Kudos to the agency. Mistakes will be made, and it’s a great idea to fix them. But it is also instructive to see where the policy was on March 4, when TIME ran a story on how the CDC was having to combat widespread public demand for masks. There had been a retail run on masks, wiping out inventories at stores, Amazon and everywhere else; many healthy people were ignoring the request not to mask up in public; celebrities like Gwyneth Paltrow and Bella Hadid were posting their pix online. And here’s the chilling part, and it’s sadly symptomatic: the magazine fully took the agency’s side on the science and had no trouble finding additional expert authority to suppress the urge to investigate. Instead, the issue was settled by decree and then embellished as factual necessity:
“It seems kind of intuitively obvious that if you put something—whether it’s a scarf or a mask—in front of your nose and mouth, that will filter out some of these viruses that are floating around out there,” says Dr. William Schaffner, professor of medicine in the division of infectious diseases at Vanderbilt University. The only problem: that’s not likely to be effective against respiratory illnesses like the flu and COVID-19. If it were, “the CDC would have recommended it years ago,” he says. “It doesn’t, because it makes science-based recommendations.”
About that, TIME wrote: “The science, according to the CDC, says that surgical masks won’t stop the wearer from inhaling small airborne particles, which can cause infection. Nor do these masks form a snug seal around the face.” The harm was not simply a run on supplies that would deprive health workers of necessary protective gear.
“Seriously people- STOP BUYING MASKS!” tweeted Dr. Jerome Adams, the U.S. Surgeon General, on Feb. 29. “They are NOT effective in preventing general public… Adams said that wearing a mask can even increase your risk of getting the virus.
This extended into the psychological realm:
Lynn Bufka, a clinical psychologist and senior director for practice, research and policy at the American Psychological Association, suspects that people are clinging to masks for the same reason they knock on wood or avoid walking under ladders. “Even if experts are saying it’s really not going to make a difference, a little [part of] people’s brains is thinking, well, it’s not going to hurt. Maybe it’ll cut my risk just a little bit, so it’s worth it to wear a mask,” she says. In that sense, wearing a mask is a “superstitious behavior”…
Earth to Experts: superstitions run in multiple directions. See: the current view of the CDC as a correction of their previous one. And note the new TIME, quoting quite a different expert view on April 6.
“Now with the realization that there are individuals who are asymptomatic, and those asymptomatic individuals can spread infection, it’s hard to make the recommendation that only ill individuals wear masks in the community setting for protection, because it’s not clear who is ill and who is not,” says Allison Aiello, a professor of epidemiology at the University of North Carolina at Chapel Hill’s Gillings School of Global Public Health, who has researched the efficacy of masks.
Another conventional view that COVID-19 spread needed person-to-person contact, touching or close-in exchange (via coughing, breathing). But now it appears to be the case that the virus hangs around in the air, and that dosing (how much you inhale) matters greatly. A well person who encounters a passing microbe might catch a mild case of COVID-19, whereas sitting next to an infected person for five hours on a bus or airplane will trigger severe infection. In this environment, the logic for masks swells.
Scientific inquiry continues. The World Health Organization posted (March 27) that there was insufficient evidence to say whether COVID-19 travels airborne for any distance. What is the action take-away? Nature (April 2) puts the state of debate like this:
[E]xperts that work on airborne respiratory illnesses and aerosols say that gathering unequivocal evidence for airborne transmission could take years and cost lives. We shouldn’t “let perfect be the enemy of convincing”, says Michael Osterholm, an infectious-disease epidemiologist at the University of Minnesota in Minneapolis. “In the mind of scientists working on this, there’s absolutely no doubt that the virus spreads in the air,” says aerosol scientist Lidia Morawska at the Queensland University of Technology in Brisbane, Australia. “This is a no-brainer.”
Nature notes that those working in the area recommended masks as a policy response.
Challenge the orthodoxy of the expert class, encourage intellectual diversity
Challenging orthodoxy is key to science; how else are errors uncovered or innovations discovered? On the frontiers there cannot be utter consensus. If there is, the thinkers have yet to probe nearly far enough. Safi Bakhall, in his remarkable Loonshots: Nurturing the Crazy Ideas that Win Wars, Cure Diseases and Transform Industries (2019), quotes Nobel Laureate in Medicine, Sir James Black: “it’s not a good drug unless it’s been killed at least three times” (45). The history of progress is pocked with failure, dispute, and persistence. Only then does a great breakthrough survive the Three Deaths.
Professor Zeynep Tufekci, of Information Sciences at the University of North Carolina, came to see her research to suggest that lives could be saved by the mass market adoption of simple, non-medical masks in the United States. She broke the ice on the N.Y. Times op-ed page with her March 17 gem: “Why Telling People They Don’t Need Masks Backfired: To help manage the shortage, the authorities sent a message that made them untrustworthy.”
Dr. Zeynep Tufekci, a professor of information science who specializes in the social effects of technology.
She put pieces of the puzzle together and made rational comparisons:
[P]laces like Hong Kong and Taiwan that jumped to action early with social distancing and universal mask wearing have the pandemic under much greater control, despite having significant travel from mainland China. Hong Kong health officials credit universal mask wearing as part of the solution and recommend universal mask wearing. In fact, Taiwan responded to the coronavirus by immediately ramping up mask production.
I’d wager Zeynep deserves a promotion, if not a Medal of Freedom. Because the fear is that this sort of commentary in the public forum will spark the opposite reaction. She believed, based on her scholarly study, that mass mask adoption might save lives, but cost her own, academically speaking. In a nifty interview with tech explainer Ben Thompson published April 2 on Stratechery,[2] Zeynep confides in how her thinking progressed.
I watched somewhat flabbergasted over the next few months as the recommendation not to wear masks got harder and harder. Instead of getting softer as the epidemic became a pandemic and saying, well, we should see, we should reevaluate, I started seeing all these messages, like people wouldn’t know how to wear masks and they would infect themselves more and also there is a big shortage of masks, and that all came together in a very frustrating moment for me. The idea that people wouldn’t figure out how to wear a surgical mask or N95s, which are those medical grade masks that we’re now reserving only for hospitals and medical workers, is kind of ridiculous. People don’t wash their hands correctly either, right? So when the pandemic hit, we have songs to get people to wash them for the right amount and we teach them how, people can obviously learn how to wear masks correctly. And as you know, people in Hong Kong can do it, in Taiwan can do it.
But I wanted somebody else from the medical fields to write this. I wanted an epidemiologist, I wanted a virologist to come out and say, look, all these health authorities in Hong Kong and Taiwan, in South Korea, in Japan where it’s kind of customary, there are all these places with lower spread… You don’t even know if you’re sick, so the recommendation of wear this if you’re sick made no sense.
So here’s how I came to write it, even though it wasn’t my place to write this, and I really kind of dragged my foot a little bit, because… I’m not an epidemiologist. I don’t have a degree in virology, I’m not the person: I wrote it because none of the doctors could write it…. I said we have to talk about this, we have to change this conversation… So I wrote the piece pretty much making the case against what was then the CDC and the World Health Organization guidelines, and I braced for the biggest backlash of my life… and I thought, I’m going to get in so much trouble over this, I’m going to be canceled, I’m going to have the huge backlash… I thought this might be the end of my writing career as I knew it… but I just have to say this, I have to say my truth.
I hope Zeynep remains asymptomatic. No – actually, I hope she is a star. If she survives and flourishes, maybe diversity of thought, and alert empirical analysis, comparing realistic options during real-time social stress, can make a splash. If so, I hope it becomes airborne.
[1] The term is attributed to Amazon CEO Jeff Bezos in Brad Stone, “The Everything Store: Jeff Bezos in the Age of Amazon” (2013). It refers to the tendency of any organization, particularly large and complicated ones, to reflexively dismiss new ideas and their sources. It is a twist on the classic NIH (Not Invented Here) problem.
[2] Subscription-required – I recommend it.